Interventional Analytics in SNFs Leads to Reduced Readmissions

This article was originally featured in Healthcare IT Today.
Bridging the data gap between acute care and post-acute care is a significant challenge. However, more and more evidence suggests that sharing the right information from acute care with post-acute care settings, like Skilled Nursing Facilities (SNFs), leads to remarkable outcomes that benefit acute care providers, SNFs, and most importantly, the patient. While it may seem obvious that sharing data between these organizations is beneficial, there is now concrete evidence to support its value.
We first highlighted some of these benefits in our previous article, The Value of Bridging the Data Gap Between Acute and Post-Acute Care at St. Joseph’s Health. To further this discussion, let’s take a look at the study in the American Journal of Managed Care, titled “Interventional Analytics in Skilled Nursing Facilities Associated with Reduced Readmissions”.
This study examined the 30-day risk-adjusted readmission rates in SNFs associated with Penn Medicine’s Lancaster General Hospital (LGH). One group of SNFs had implemented an interventional analytics solution from Real Time Medical Systems (Real Time), while the other group had not. The study also utilized CMS SNF quality performance data to compare LGH’s readmission rates with those of other organizations at both the state and national levels.
Over the course of the study period from 2017-2022, LGH showed lower readmission rates than other healthcare organizations in Pennsylvania and throughout the United States. However, after the implementation of the interventional analytics solution that provided real-time data analysis to the SNFs, those facilities that utilized this actionable information saw a greater reduction in readmissions. In fact, the study found that readmission rates were 15.24%, 12.30%, and 13.06% points lower for SNFs using the interventional analytics compared to those who did not, the Pennsylvania cohort, and the national cohort, respectively.
Here’s a look at the charts showing the readmission rates for the different cohorts studied:
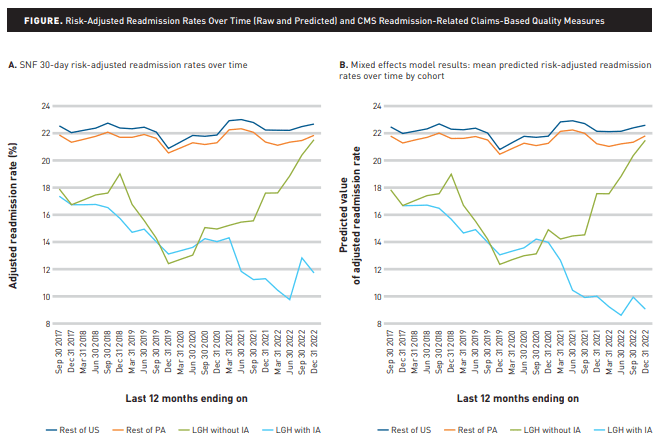
As you can see, the light blue line highlights the significant reduction in readmissions at the LGH SNFs that utilized the interventional analytics from Real Time.
What’s particularly interesting about this study is that it also analyzed other CMS readmission-related claims-based quality measures to see how they compare across the various cohorts. For SNFs that utilized the interventional analytics, the data showed a reduction in Medicare spending per beneficiary, a decrease in hospitalizations due to infections acquired during the SNF stay, and an increase in the rate of successful transitions back to home or community settings.
I love to see these tangible outcomes resulting from having the right data in the right place at the right time. Although, what likely warrants further analysis is identifying which specific data was key to producing these results. There are many healthcare interoperability solutions available that share significant amounts of data between healthcare organizations. However, overwhelming clinicians with a large amount of data is unlikely to address the issue. For data to be truly useful, it must be transformed into actionable insights.
This is why I appreciate that this study focused on interventional analytics. While a platform that provides access to health data is beneficial, an interventional analytics platform that connects data to relevant interventions is far more impactful and seems crucial for achieving results like those seen in the study.
As the study highlights, there were approximately 1.7 million SNF admissions in the United States in 2018, with 22% of those patients being readmitted to the hospital within 30 days of their SNF admission. That amounts to 377,000 patients being readmitted to the hospital. Additionally, the study estimates that these readmissions cost Medicare $5.2 billion dollars. Implementing solutions like Real Time’s interventional analytics, as discussed in this study, could significantly improve patient outcomes and reduce healthcare costs, potentially representing annual savings of $2.8 billion dollars for CMS.
Check out the full study for all the details: Interventional Analytics in Skilled Nursing Facilities Associated with Reduced Readmissions.
You may view this article on the Healthcare IT Today website, here.