How Technology Drives Value-Based Care
This article was originally featured in Healthcare IT Today.
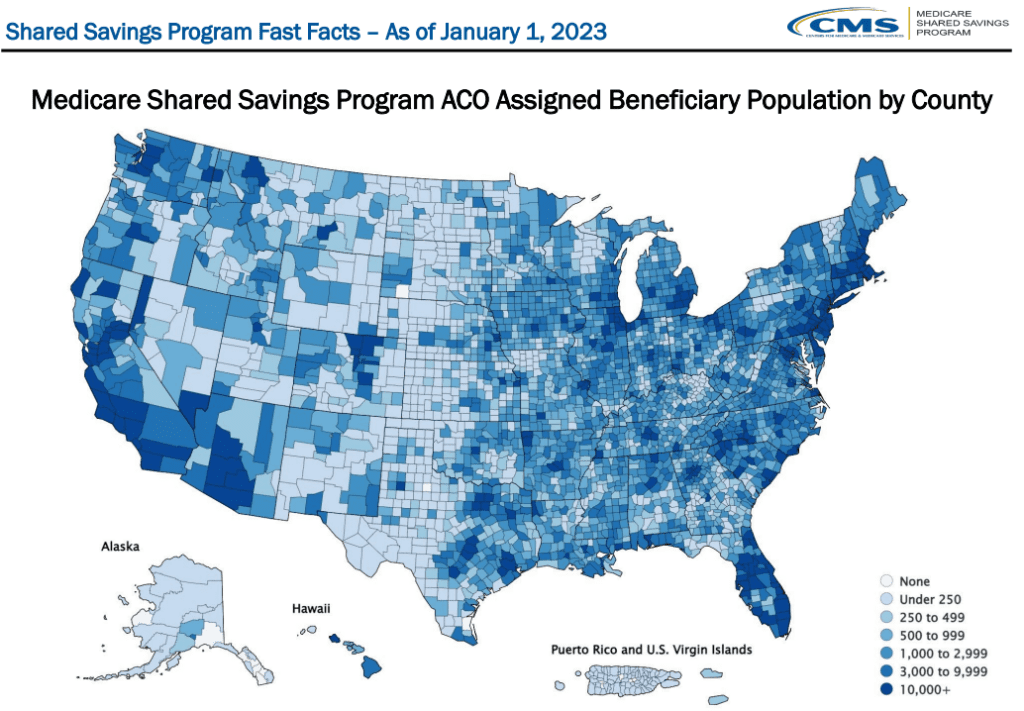
We all know that CMS is pushing hard towards value-based care. Their goal is to have 100% of Medicare beneficiaries in a value-based care arrangement by 2030. We see a number of ACO approaches that make up these efforts, along with Medicare Advantage plans. While there are a lot of nuances to their approaches to value-based care, at the core of each of them, is the technology that allows healthcare organizations to make value-based care a reality. Without the right technology, is value-based care even possible?
Another thing we’ve learned over the years, is that it’s generally not possible to address value-based care alone. You have to leverage a network of providers to address the health of the populations you serve, and it takes technology to allow these organizations to connect and collaborate. Otherwise, you’re not going to drive the savings needed to be successful. Plus, when it comes to savings, many acute care organizations have rung the proverbial sponge as much as they can when it comes to changes they can make internally, such as length of stay and hospital readmissions. Sure, they may be able to get a little more out of their efforts, but it’s time for providers to collaborate with other care partners and utilize technology to be successful in value-based care.
One of the biggest areas of opportunity within value-based care is working with skilled nursing facilities (SNFs) and other post-acute organizations. Unfortunately, as it stands today, most referrals to post-acute care happen in a literal black box. The referral is made, and the patient arrives at a SNF without the right information being communicated. Not to mention, it is even more rare for the information from a SNF to be communicated back to the referring care facility. The post-acute EHR software out there isn’t passing the right information amongst care facilities during patient transitions. How can you effectively manage a patient’s care in your pool of value-based care populations at a SNF if the referring provider doesn’t have visibility into what’s happening there? You can’t.
When you dive into this more, you can see all sorts of value-based care opportunities by providing the right information from SNFs and post-acute providers to ACOs and other acute care organizations. The referring provider often sends the patient to a SNF with a specific clinical pathway in alignment with care standards for that patient to properly heal from their condition. But how does the referring facility know if clinical standards of care are being followed? Unfortunately, faxes don’t solve this problem. However, the right technology can provide visibility into a patient’s care at the SNF, allowing the referring provider to know how their doing in real-time.
There is also something even more powerful that can happen when the acute care provider has visibility into their post-acute patients. With access to live patient data, care providers can see changes to a patient’s health immediately, allowing for an opportunity to intervene in care before an adverse event occurs. Technology can ensure the right information is being shared, with the right people, at the right time. Sharing information amongst providers allows for time to intervene in care before it becomes a larger issue and hurts their value-based care efforts. The reality is that SNFs are experts on rehabilitating patients and acute care is great at treating clinical conditions. In order to be successful in value-based care, we have to combine those expertise to be able to improve patient care and outcomes.
In value-based arrangements like an ACO, you have to figure out how you can care for the patient in whatever setting they may be in. Whether that is in the hospital, at home, or in a post-acute facility. Early interventions are the best way to prevent patients from going back to the hospital for care that would not be needed if the right care had been provided earlier. Plus, having technological connections can also ensure that patients are following their treatment plan in alignment with clinical standards, helping to meet appropriate quality metrics.
An example of intervening in care early to prevent an adverse event from occurring is when a patient is being transferred to a SNF. The first three days at a SNF are when they are at higher risk for a readmission. This is largely due to what we call transition of care errors. One approach to solving these problems is ensuring that the right information on the patient is communicated to the SNF, before they arrive at the facility. However, we know that does not always happen or there is a significant lag time from when the patient information was sent and when the SNF needs it.
While this proactive sharing of information is great and should happen much more efficiently than it does today, there is another way to avoid these transition of care errors. That is through visibility into the patient care being provided by the SNF. By doing so, the ACO or acute care provider can see when a medication may not be being administered at the SNF. Once they see that, they can learn if the staff knows about the medication or possibly if there’s a medication shortage that does not allow the SNF to get it, but the hospital could if they had only known. Providing the right information to the right people can improve this problem.
I saw another example of this in action when referring providers were upset with a SNF that was waiting two days to provide rehab care to a patient after repairing a fractured hip. It was understandable that the care teams were frustrated since they had worked so hard with the patient to help them recover, just to have the lack of rehab impact recovery after being referred to a post-acute provider. Additionally, the delay in rehab meant extra costs, impacting their value-based care efforts. Without visibility between acute and post-acute care, this would have been a frustrating situation with no remedy.
In this instance, acute and post-acute care partnered together, sharing data from the SNF. From that collaboration, they were able to discover that patients were being given a narcotic which was causing them to have urinary retention at the SNF. This condition makes rehab no longer possible. The clinical team realized that if they switched to a slightly more expensive medication vs. the narcotic, they could avoid this issue and rehab could start quickly after arriving at the SNF. The right technology brought these providers together to improve the patient experience, and their value-based care efforts overall, despite using a more expensive medication.
These examples point out how important it is to have a true technological collaboration between acute and post-acute care providers. Rather than pointing fingers at each other, technology can help providers collect and share the right data across their network, understanding what changes need to be done to improve the quality of care the patient receives.
With a few exceptions, most value-based care arrangements pay the doctor or acute care organization – not the SNF. However, the actions the SNF takes often impacts your value-based care efforts as much as anything else. It is time that ACOs and other acute care providers share some of the savings they achieve thanks to their post-acute care partners. Plus, SNFs need to embrace these partnerships as well, since doing so can save them the manual efforts for things like regulatory reporting. The data that ACOs need is often the same information that has to be reported to regulatory bodies. Furthermore, a SNF that’s providing the highest quality, low cost care is going to drive more volume to their organization from the referring facilities.
You may view this article on the Healthcare IT Today website, here.